Applying Denial Management to Build Value And Improve Revenue!!
What is Denial?
Denial of a claim is the refusal of an insurance company, or carrier to honor a request by an individual, his or her provider, to pay for healthcare services obtained from a healthcare professional.

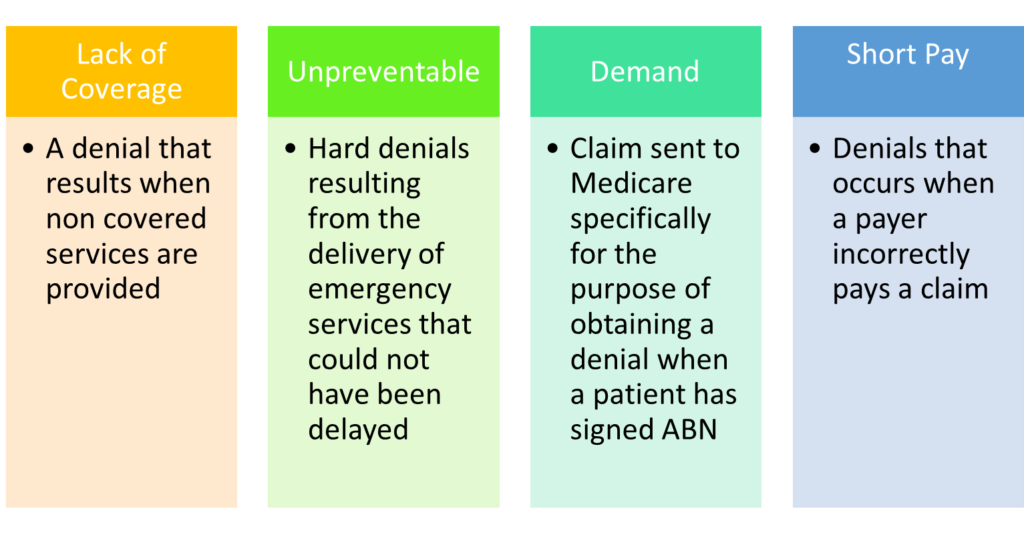
What are the Denial Types?
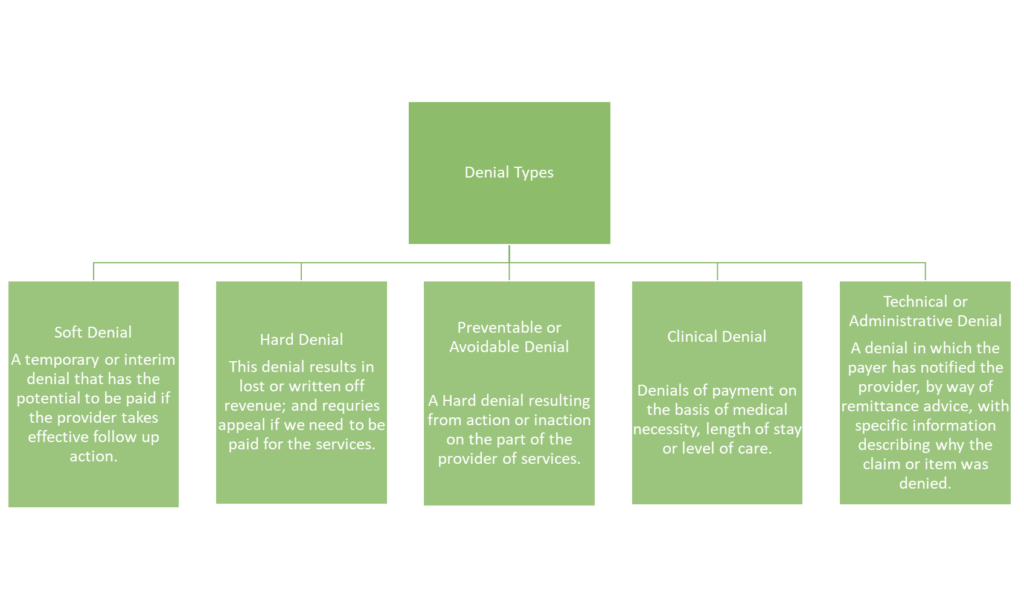
Misclassified Denials
Denial Management is one the most important piece of Revenue Cycle Management in Healthcare. The rate at which medical claims get denied by insurers is pretty concerning. According to recent research, the average claim denial rate is increased by 23 percent as compared to four years ago.
For medical practices, increased claim denials mean unpaid services, resulting in lost or delayed revenues, hurting the financial health tremendously.
To ensure a healthy cash flow, healthcare organizations need to focus mainly on the root cause and denial prevention.
It is also important to note that, the term Claim Denial and Claim Rejection are often used interchangeably as they both might be a part of Denial Management Processes.
However, they are not the same.
Rejected claims will not be processed as they have not been received/accepted by the payer, therefore these claims do not make it into the adjudication system and they need to be resubmitted once the errors have been corrected. It is commonly observed that this reduces the cash flow, as no one is looking at the system rejecting reports and ends up overlooking the same.
A denied claim, on the other hand, has been received by the payer and has been adjudicated and payment determination has already been processed.
A denied claim has been determined by the insurance company to be unpayable. Denied claims represent unpaid services and lost or delayed revenue to the practice.
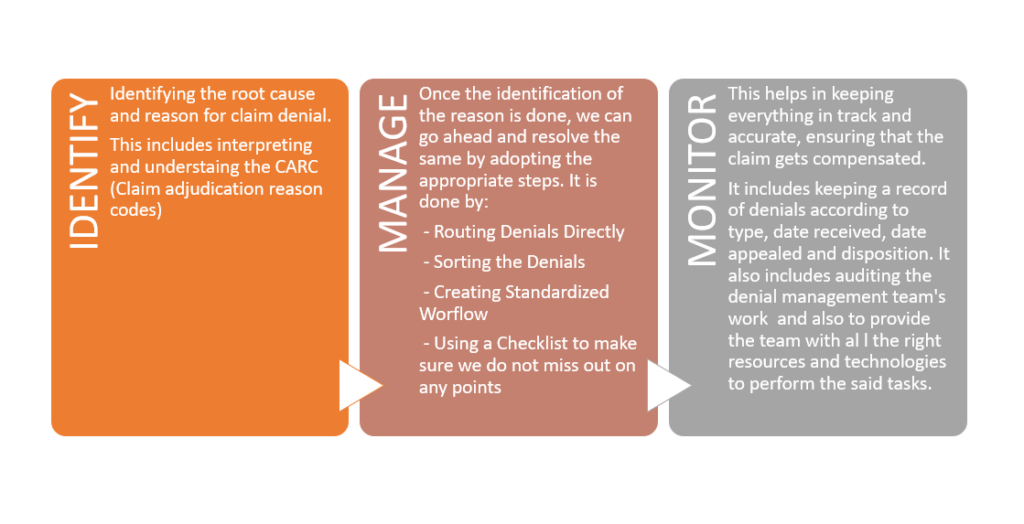
Denial Management thus can be defined as a Strategic Process that aims to unveil and resolve problems leading to medical claim denials. The process also helps in mitigating the risk of future denials, ensuring best practices get paid faster, and helps in maintaining a healthy and steady cash flow.
A trend analysis is done by the Denial Management team checking the recurring denial reason codes and denial reason codes. The whole idea around it is to point out the registration, billing, and medical coding setbacks through trend tracking and using corrective plans to reduce the same in the future.
The team also helps with analyzing the payment patterns for individual payers so that it becomes effortless to detect a diversion from the normal trend.
What is IMMP Process and How Does it help with Denial Management?
Why do we require Denial Management in a Healthcare Organization?
Ensuring your claims are complete, correct, and able to be processed by the insurance company is an achievement on its own, as it saves the organization from potential revenue loss.
It also helps in maintaining processes that can help in maintaining hygiene for future denials.
A denial management plan/system helps in timely tracking, prioritizing, and appealing denials based on case citations and state/federal statutes supporting the entity’s appeal.
Collecting and analyzing denials patterns unmasks their root cause, enabling the denial management team to devise a permanent solution for such categories.
Denial management also allows a healthcare organization to collect more candid information to support the appeal, which also helps in increasing the claim amount.
What is StatusNeo’s role in Denial Management?
We understand each denial case is unique.
We correct invalid or incorrect medical codes, provide supporting clinical documentation, appeal any prior authorization denials, understand any genuine denial cases to pass the responsibility to patients, and follow up effectively.
StatusNeo has helped major Healthcare Providers by reducing denials through analytics.
Different component processes within the revenue cycle chain can result in claim denials. Often, denial issues are practice-specific or facility-specific. We understand the trends in claim denials and launch an iterative process to reduce them based on specific causes.
Our team of highly qualified and experienced members have effectively reduced the denial percentage, thereby, increasing, and stabilizing the Healthy cash flow.
References:
https://www.mgsionline.com/healthcare-denial-management.html
Add Comment
You must be logged in to post a comment.